A little over a year ago, Joseph Coates was told there was only one thing left to decide. Did he want to die at home, or in the hospital?
Coates, then 37 and living in Renton, Wash., was barely conscious. For months, he had been battling a rare blood disorder called POEMS syndrome, which had left him with numb hands and feet, an enlarged heart and failing kidneys. Every few days, doctors needed to drain liters of fluid from his abdomen. He became too sick to receive a stem cell transplant — one of the only treatments that could have put him into remission.
“I gave up,” he said. “I just thought the end was inevitable.”
But Coates’s girlfriend, Tara Theobald, wasn’t ready to quit. So she sent an email begging for help to a doctor in Philadelphia named David Fajgenbaum, whom the couple met a year earlier at a rare disease summit.
By the next morning, Dr. Fajgenbaum had replied, suggesting an unconventional combination of chemotherapy, immunotherapy and steroids previously untested as a treatment for Coates’s disorder.
Within a week, Coates was responding to treatment. In four months, he was healthy enough for a stem cell transplant. Today, he’s in remission.
The lifesaving drug regimen wasn’t thought up by the doctor, or any person. It had been spit out by an artificial intelligence model.
In labs around the world, scientists are using A.I. to search among existing medicines for treatments that work for rare diseases. Drug repurposing, as it’s called, is not new, but the use of machine learning is speeding up the process — and could expand the treatment possibilities for people with rare diseases and few options.
Thanks to versions of the technology developed by Dr. Fajgenbaum’s team at the University of Pennsylvania and elsewhere, drugs are being quickly repurposed for conditions including rare and aggressive cancers, fatal inflammatory disorders and complex neurological conditions. And often, they’re working.
The handful of success stories so far have led researchers to ask the question: How many other cures are hiding in plain sight?
There is a “treasure trove of medicine that could be used for so many other diseases. We just didn’t have a systematic way of looking at it,” said Donald C. Lo, the former head of therapeutic development at the National Center for Advancing Translational Sciences and a scientific lead at Remedi4All, a group focused on drug repurposing. “It’s essentially almost silly not to try this, because these drugs are already approved. You can already buy them at the pharmacy.”
The National Institutes of Health defines rare diseases as those which affect fewer than 200,000 people in the United States. But there are thousands of rare diseases, which altogether affect tens of millions of Americans and hundreds of millions of people around the world.
And yet, more than 90 percent of rare diseases have no approved treatments, and pharmaceutical giants don’t commit many resources to try to find them. There isn’t typically much money to be made developing a new drug for a small number of patients, said Christine Colvis, who heads drug development partnership programs at NCATS.
That’s what makes drug repurposing such “an enticing alternative” route to finding treatments for rare diseases, said Dr. Marinka Zitnik, an associate professor at Harvard Medical School who studies computer science applications in medical research. Dr. Zitnik’s Harvard lab has built another A.I. model for drug repurposing.
“Other laboratory discovery techniques have already put drug repurposing on the map,” Dr. Lo said. “A.I. just puts rocket boosters on that.”
Finding Clues in Old Research
Repurposing is fairly common in pharmaceuticals: Minoxidil, developed as a blood pressure medication, has been repurposed to treat hair loss. Viagra, originally marketed to treat a cardiac condition, is now used as an erectile dysfunction drug. Semaglutide, a diabetes drug, has become best known for its ability to help people lose weight.
The first time Dr. Fajgenbaum repurposed a drug, it was in an attempt to save his own life. At 25, while in medical school, he was diagnosed with a rare subtype of a disorder called Castleman disease, which led to an immune system reaction that landed him in the intensive care unit.
There is no one way to treat Castleman disease, and some people don’t respond to any of the available treatments. Dr. Fajgenbaum was among them. Between hospitalizations and rounds of chemo that temporarily helped, Dr. Fajgenbaum spent weeks running tests on his own blood, poring over medical literature and trying unconventional treatments.
“I had this really clear realization that I didn’t have a billion dollars and 10 years to create some new drug from scratch,” he said.
The drug that saved Dr. Fajgenbaum’s life was a generic medication called sirolimus, typically given to kidney donation recipients to prevent rejection. The medication has kept his Castleman disease in remission for more than a decade.
Dr. Fajgenbaum went on to become a professor at the University of Pennsylvania, and began seeking out other drugs with unknown uses. Existing research, he realized, was full of overlooked clues about potential links between drugs and the diseases they could treat, he said. “If they’re just in the published literature, shouldn’t someone be looking for these all day, every day?”
His lab had some early successes, including finding that a novel cancer drug helped another Castleman patient. But the process was laborious, requiring his team to examine “one drug and one disease at a time,” he said. Dr. Fajgenbaum decided he needed to speed up the project. In 2022, he established a nonprofit called Every Cure, aimed at using machine learning to compare thousands of drugs and diseases all at once.
Work similar to Every Cure’s is taking place in other labs around the world, including at Penn State and Stanford University, as well as in Japan and China.
In Birmingham, Ala., an A.I. model suggested a 19-year-old patient debilitated by chronic vomiting try isopropyl alcohol, inhaled through the nose. “Essentially we ran a query that said, ‘Show us every proposed treatment there has ever been in the history of medicine for nausea,’” said Matt Might, a professor at University of Alabama at Birmingham who leads the institute that developed the model.
The alcohol “popped to the top of our list,” Dr. Might said, and “it worked instantly.”
The model developed by Dr. Might’s institute has successfully predicted other treatments, too: Amphetamines typically used to treat A.D.H.D. relieved periodic paralysis in children with a rare genetic disorder. A Parkinson’s drug helped patients with a neurological condition move and speak. A common blood pressure medicine called guanfacine drastically improved the mobility of a pediatric patient with a different neurological condition.
Many drugs do more than one thing, Dr. Might said. Their additional features sometimes get characterized as side effects. “If you comb through enough drugs, you eventually find the side effect you’re looking for,” he said, “and then that becomes the main effect.”
At the University of Pennsylvania, Dr. Fajgenbaum’s platform compares roughly 4,000 drugs against 18,500 diseases. For each disease, pharmaceuticals get a score based on the likelihood of efficacy. Once the predictions are made, a team of researchers combs through them to find promising ideas, then performs lab tests or connects with doctors willing to try the drugs on patients.
Elsewhere, pharmaceutical companies are using A.I. to discover entirely new drugs, a pursuit that has the potential to streamline an enterprise already worth billions. But drug repurposing is not likely to prove lucrative for any one party. Many drug patents expire after a few decades, which means there is little incentive for drug companies to seek out additional uses for them, said Aiden Hollis, a professor of economics at the University of Calgary with a focus on medical commerce.
Once a drug becomes one of the thousands of generics approved by the Food and Drug Administration, it typically faces stiff competition, driving down the price.
“If you use A.I. to come up with a new drug, you can make lots and lots of money off that new drug. If you use A.I. to find a new use for an old, inexpensive drug, no one makes any money off of it,” Dr. Fajgenbaum said.
To fund the venture, Every Cure received more than $100 million in commitments last year from TED’s Audacious Project and the Advanced Research Projects Agency for Health, an agency within the federal health department dedicated to supporting potential research breakthroughs. Dr. Fajgenbaum said that Every Cure will use the money, in part, to fund clinical trials of repurposed drugs.
“This is one example of A.I. that we don’t have to fear, that we can be really excited about,” said Dr. Grant Mitchell, another Every Cure co-founder and a medical school classmate of Dr. Fajgenbaum. “This one’s going to help a lot of people.”
‘Someone Had to Be The First to Try’
Dr. Luke Chen was skeptical when Dr. Fajgenbaum’s model suggested he treat a patient with Castleman disease using adalimumab, a medication typically used to treat arthritis, Crohn’s disease and ulcerative colitis.
“I didn’t think it was going to work, because it’s kind of a wimpy drug,” said Dr. Chen, a hematologist and professor at Dalhousie University and the University of British Columbia.
But the patient had already undergone chemotherapy and a bone-marrow transplant and had tried drugs including the one that saved Dr. Fajgenbaum’s life. Nothing worked, and he was entering hospice.
“We had basically given up, but I put in a last call to David,” Dr. Chen said.
With no other options, Dr. Chen gave the patient the adalimumab. In a matter of weeks, the patient was in remission. The case was recently the subject of a paper in The New England Journal of Medicine.
No model is infallible, Dr. Zitnik said. A.I. can sometimes make predictions “based on evidence that isn’t sufficiently strong.”
Dr. Colvis said ranking potential treatments by likelihood of success can also prove difficult. Such issues make physician oversight crucial. Sometimes, a doctor will determine that a treatment suggestion is too risky to try, she said. “But then there are instances where they will see something and say, ‘OK, this looks like it’s reasonable,’” Dr. Colvis added.
When Dr. Fajgenbaum first suggested that Dr. Wayne Gao, a hematologist and oncologist in Washington State, try a novel treatment on one of his patients, Dr. Gao had doubts.
The patient was Coates, the Washington man headed for hospice, and the aggressive drug combination suggested by Dr. Fajgenbaum’s model seemed “a little bit crazy,” Dr. Gao said. In fact, he worried that the treatment might kill Coates faster.
But Coates was a young man, and there were no other treatments to consider. And so, Dr. Gao said, “someone had to be the first to try.”
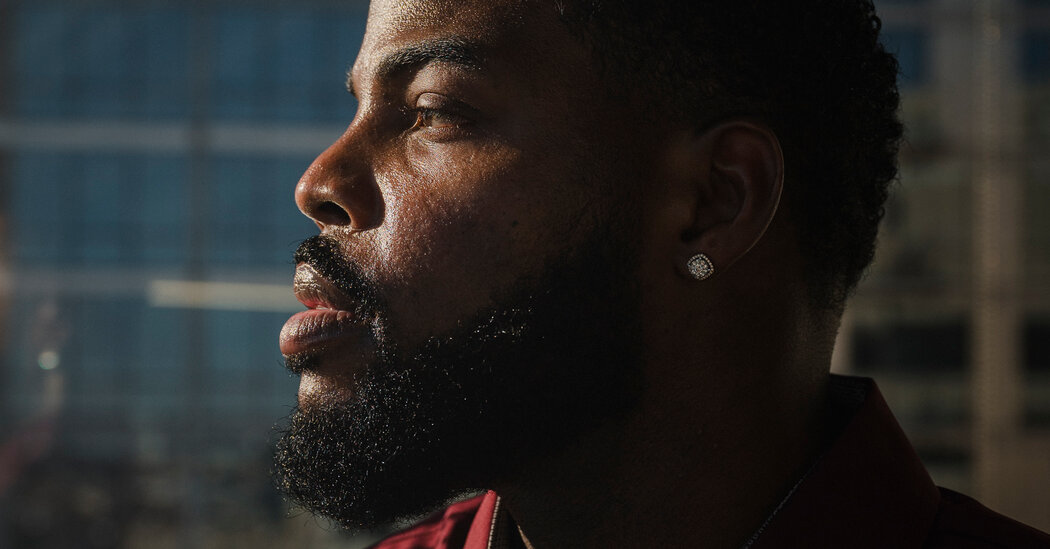
Last month, just over a year after his brush with death, Coates and his girlfriend visited Dr. Fajgenbaum in Philadelphia to thank him for his help. A smiling Coates was the picture of health; he had put on muscle since the last time he met the doctor.
Coates had tweaked his ankle that morning while working out. But otherwise, he said, he felt “just fine.”
Maxwell Strachan contributed reporting.